Recognise symptoms early and ask your HCP to listen to your heart
Diagnosis journey for aortic stenosis patient

Stage 1
HCP listens to your heart1
Stage 2
You are referred for an echocardiogram2
Stage 3
You are monitored by HCP2
Stage 1
A healthcare professional listens to your heart1
Aortic stenosis can start off mild and then slowly progress until the heart fails. During the early stages of the condition, you may have few, if any, symptoms.3
Aortic stenosis causes the aortic valve in your heart to narrow over time, making the heart work harder to pump blood out to the rest of the body. The damage to the valve changes the noise your heart makes as it beats.4,5
The healthcare professional will listen for a heart murmur, because this could be a sign of aortic stenosis.4,5 If a heart murmur is detected, the GP should refer you for further tests to find out what is happening.1

If you experience symptoms, such as breathlessness, chest pain and fatigue, ask a healthcare professional to listen to your heart using a stethoscope.4
Stage 2
You are referred for an echocardiogram2
If your healthcare professional suspects a heart murmur, you should be referred for an echocardiogram as soon as possible.2
The healthcare professional who performs the echocardiogram will also listen to your heart using a stethoscope to confirm the heart murmur, but an echocardiogram is key to confirming the diagnosis and severity of aortic stenosis.2,3,4
An echocardiogram is a painless procedure that uses ultrasound to scan your heart. A probe is passed over the chest and sends out high-frequency sound waves that bounce off the heart. The echoes are picked up by the probe and displayed on a screen.6
A diagnosis of aortic stenosis is made by measuring the size of the gap in the aortic valve:7
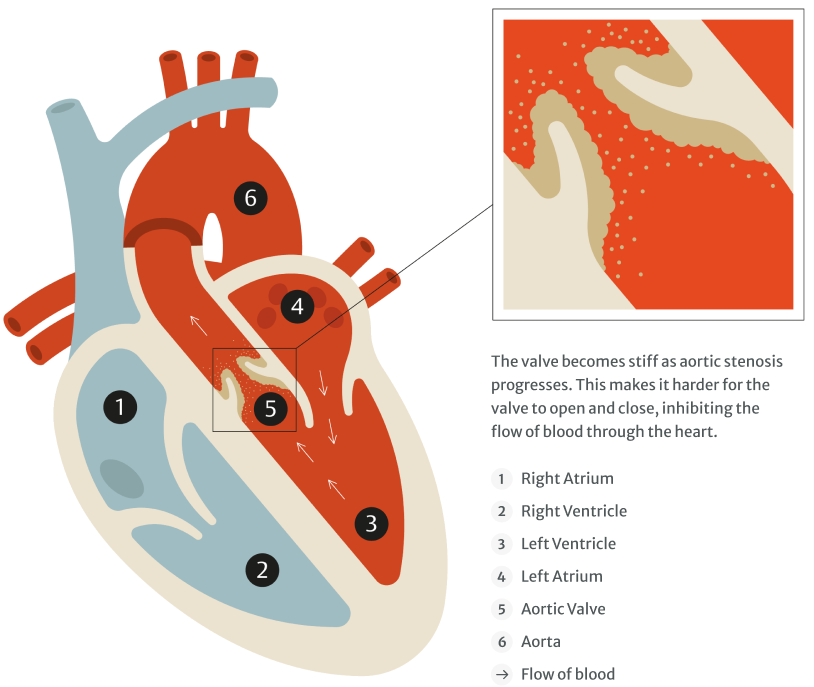

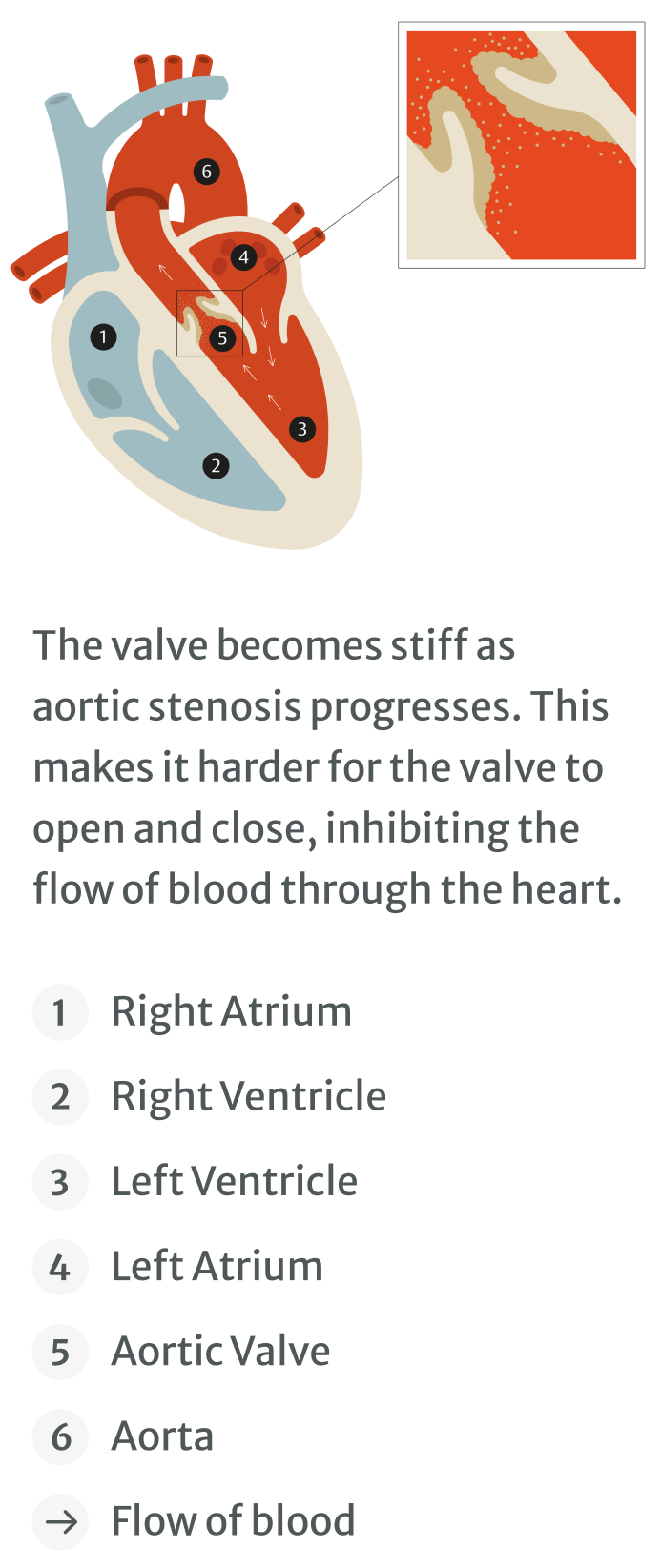
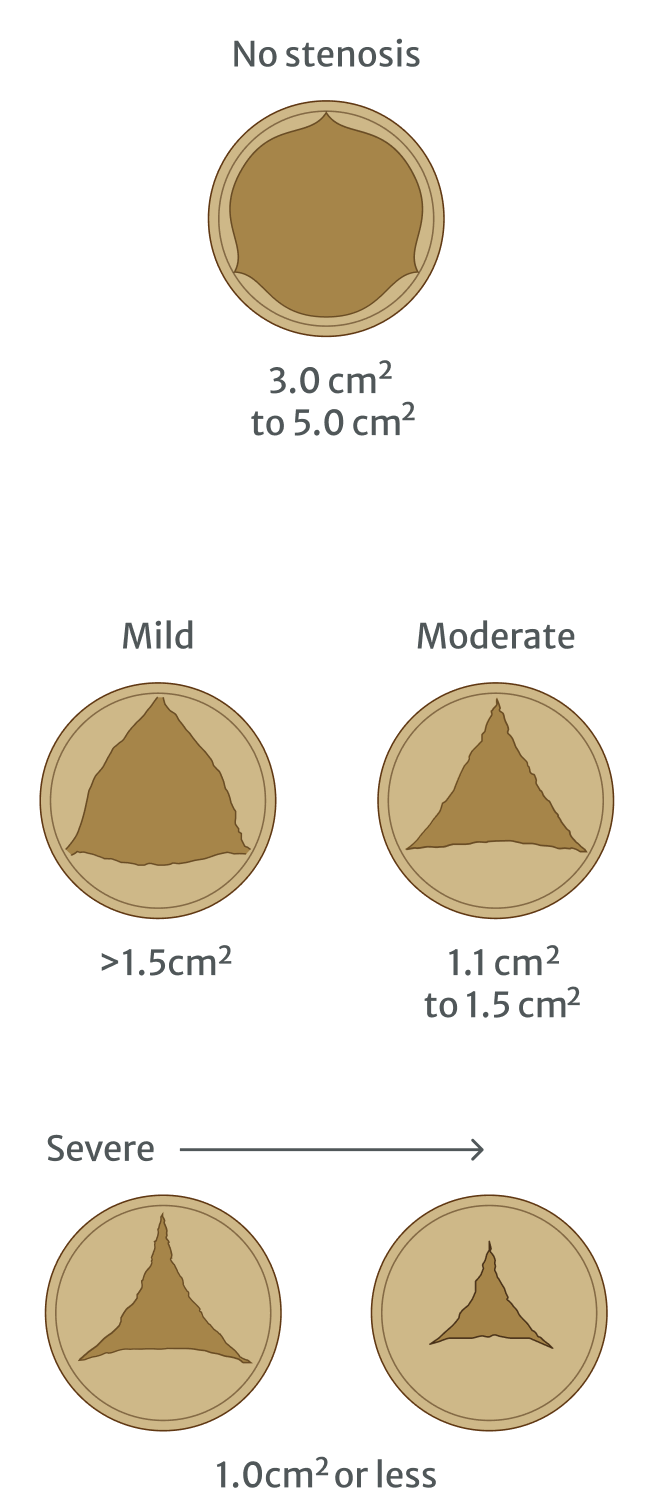
Adapted from Mayoclinic.org
Stage 3
Monitoring your aortic stenosis and what happens if it gets worse
If you have received a diagnosis of aortic stenosis and you don’t have any symptoms, it’s unlikely you will need treatment to replace the aortic valve right away. However, attending your medical appointments is very important as your healthcare professional will monitor you to see if the condition is progressing.2,8
If you start experiencing aortic stenosis symptoms, see your healthcare professional as soon as you can. You should be referred for more tests to check if your condition has progressed to a more severe stage.2,9
- People with mild aortic stenosis should have regular (every 2–3 years) assessments to monitor progression of the condition.2
- People with moderate aortic stenosis should be assessed more often (once a year).2
- People with severe aortic stenosis should have regular, 6-month assessments with a healthcare professional to monitor progression of the condition.2
The tests may include further echocardiograms or monitored exercise that can expose any hidden symptoms of aortic stenosis.2,10,11

Once you start getting symptoms of aortic stenosis, you will need to be referred to a cardiologist for further assessment and eventual treatment to replace your aortic valve.2,9
1. British Heart Foundation. Heart murmurs - Causes, Symptoms & Treatment. Available at: https://www.bhf.org.uk/informationsupport/conditions/heart-murmurs (accessed March 2022).
2. ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2021; ehab395. doi:10.1093/eurheartj/ehab395
3. Oxford University Hospitals NHS. Aortic Stenosis. Available at: https://www.ouh.nhs.uk/cardiac/services/cardiology/specialist-services/aortic-stenosis (accessed March 2022).
4. Grimard BH, Larson JM. American Family Physician. 2008;78(6):717–724.
5. Nishimura RA, et al. Journal of the American College of Cardiology. 2014;63(22):2438–2488.
6. NHS. Echocardiogram. Available at: https://www.nhs.uk/conditions/echocardiogram (accessed March 2022).
7. Mayo Clinic. Aortic valve stenosis: Symptoms & Causes. Available at: https://www.mayoclinic.org/diseases-conditions/aortic-stenosis/symptoms-causes/syc-20353139 (accessed March 2022).
8. Global Heart Hub. Heart Valve Disease: Working Together to Create a Better Patient Journey. Available at: https://globalhearthub.org/wp-content/uploads/2020/12/HeartValveReport2020.pdf (accessed March 2022).
9. National Institute of Health & Care Excellence. Guideline. Heart valve disease presenting in adults: investigation and management. Available at: https://www.nice.org.uk/guidance/ng208/documents/draft-guideline (accessed March 2022)
10. Généreux P, et al. J Am Coll Cardiol. 2016;67(19):2263—2288.
11. Redfors B, et al. Circulation. 2017;135(20):1956—1976.