How is aortic stenosis diagnosed?4
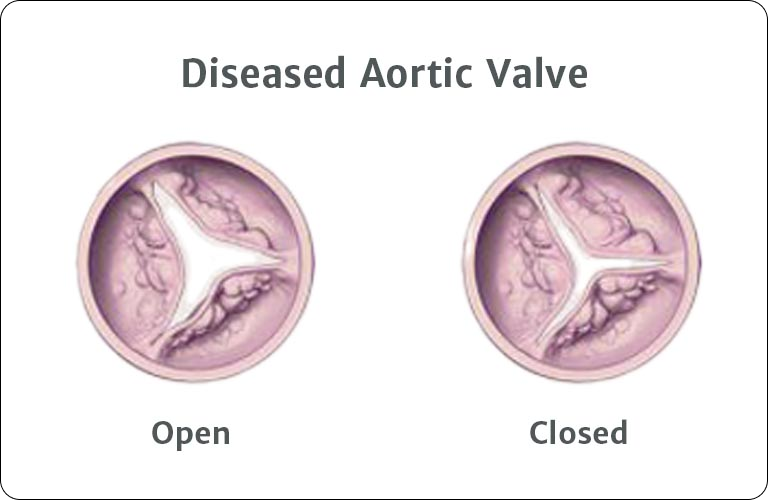
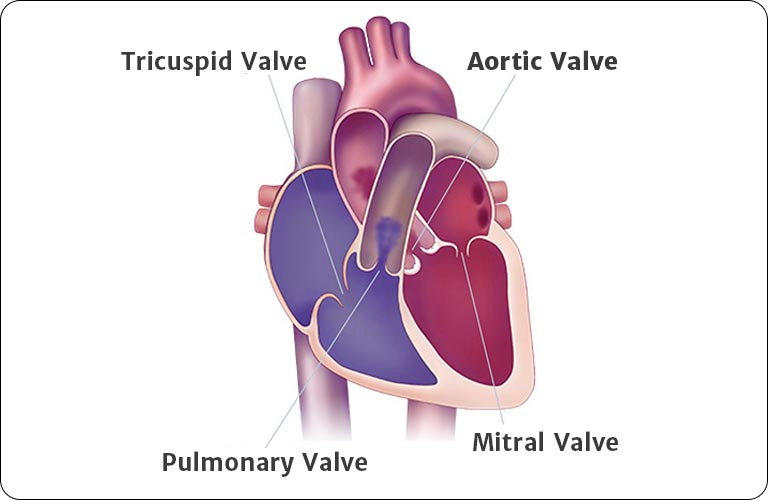
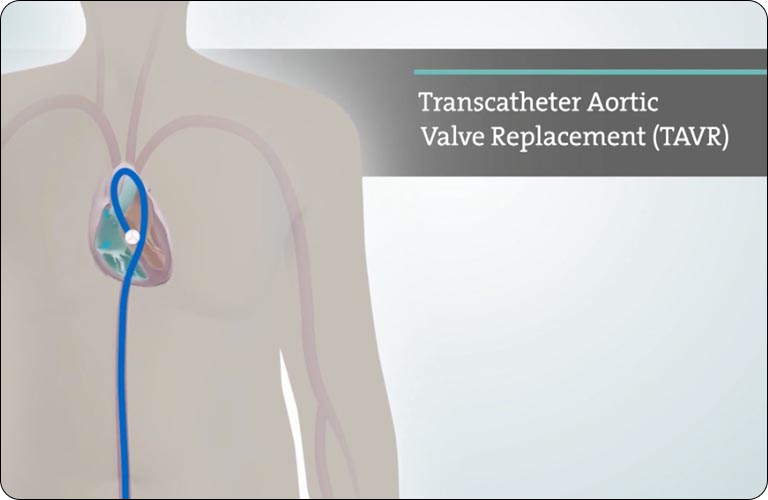
An echocardiogram (a non-invasive test that checks how well your heart valves are working) may be helpful in the diagnosis of aortic stenosis. But you shouldn’t rely solely on the test to monitor your heart health. Attending regular appointments with your doctor and communicating any changes in your daily routine, including new or worsening symptoms, is the best way to stay one step ahead of your aortic stenosis.


 Australia
Australia
 Germany
Germany
 Italy
Italy
 Netherlands
Netherlands
 South Korea
South Korea
 Southeast Asia
Southeast Asia
 United Kingdom
United Kingdom